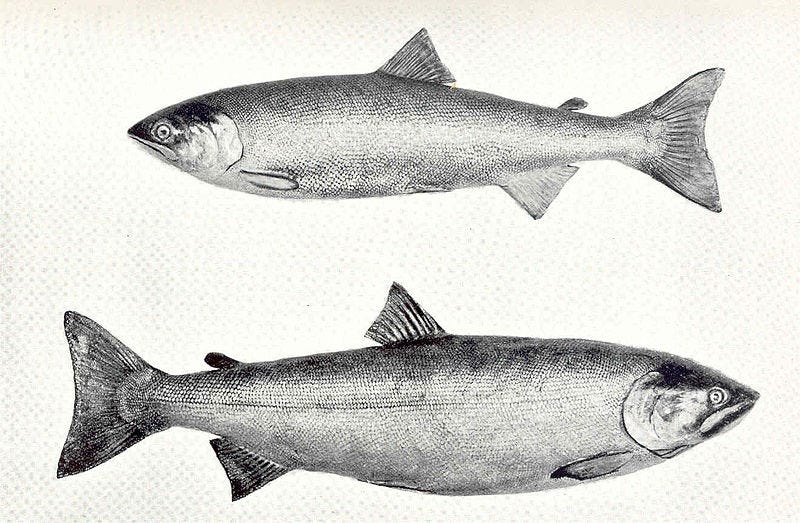
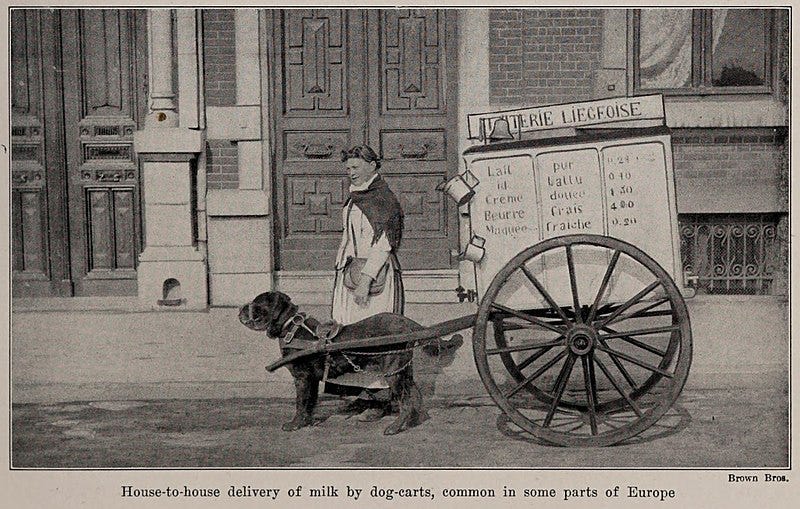
Ok…. grab a glass of milk, and some sockeye salmon, and let’s finish this thing!
In my first post on vitamin D, I went through an introduction to the hormone, how we know it’s important, and some simple ways to increase your levels through diet and modest sun exposure. Now we’re going to run through the thorny question of whether that’s enough. Do we need to take supplements? As with most things, the answer needs to be tailored to the individual… so talk to your doctor as they say. But in general, here are the considerations that will be swirling around your doc’s head as they try to give you a quick answer. That’s assuming they are keeping up with their reading, or going so far as to write a Substack?
There are medical conditions that can definitely cause low vitamin D levels. But there are also diseases that seem to be linked to low vitamin D levels such that doctors have been convinced they are caused by low D levels.
Yet there is a growing body of evidence that giving extra vitamin D paradoxically is not working to prevent things like cancer, heart problems, and autoimmune disease. It is a really hard concept for our rational brains to accept. We want to think logically: something is low, diseases are associated with that thing being low, let’s replace it, and then the diseases should be improved or even prevented.
But what we need to accept is that evidence matters the most. Is there evidence that giving vitamin D prevents, treats, or improves diseases associated with it being low? Not really.
Two phrases come to mind.
Correlation does not equal causation. Just because two things are associated, it does not prove one causes the other.
Don’t rely on “what should work,” but rather focus on “what has been shown to work.”
The following medical problems increase the risk of having a true vitamin D deficiency:
Kidney disease, psoriasis, gastric bypass surgery, celiac disease, or inflammatory bowel disease, Cystic fibrosis, obesity (fat cells keep vitamin D sequestered), liver disease, weight-loss surgeries, and certain medications that can cause vitamin D deficiency (including laxatives, steroids, cholestyramine and colestipol, phenobarbital and phenytoin, rifampin, and Orlistat).
It is also good to check D levels in people experiencing symptoms like low back pain, bone pain, muscle weakness, and muscle aches.
So what conditions have been found to be associated with low vitamin D levels? Remember, “associated” is the key word. This does not imply conclusions such as “is caused by,” “is preventable with,” or “is treatable with” vitamin D supplements.
Association studies have related vitamin D deficiency and living at higher latitudes with increased risk for many chronic diseases including autoimmune diseases, some cancers, cardiovascular disease, infectious disease, severe Covid, depression, schizophrenia and type 2 diabetes.
Vitamin D deficiency can cause or worsen osteoporosis.
Many studies have tried to improve or prevent the above conditions by giving vitamin D supplements. I could type up a book here describing them, but out of mercy for me and you, I will list some of the most recent compelling results using just a sentence or two each. Kind of like a tweet, before tweeting got ruined.
Vitamin D3 supplementation did not result in a significantly lower risk of fractures than placebo among generally healthy midlife and older adults, over a 5 year time frame of study.
For osteoporosis, exercise including aerobic and resistance activities helps prevent bone loss; exercise also helps prevent falls in older adults; calcium and vitamin D supplementation has not been shown to reduce fracture risk.
Routine supplementation in relatively healthy adults did not lower 6-year mortality.
Vitamin D supplementation does not alter cardiovascular risk, including heart attack, stroke, cardiovascular mortality, or all-cause mortality.
One study found that vitamin D reduced the risk of developing an autoimmune disease, but about 400 people would need to take the supplement to prevent one case. Nonetheless, this worked out to a 22% reduction in risk.
Vitamin D levels are not associated with risk for SARS-CoV-2 infection.
Routine use of vitamin D to treat COVID-19 patients doesn’t lower mortality or shorten length of hospital stay.
Children of pregnant women who received vitamin D at 2400 IU versus the standard recommendation of 400 IU daily showed no differences in motor, language, cognitive, emotional, or behavioral development at 6 years.
Doses of 1000 IU daily or higher did not prevent falls, and fall risk actually increased with higher doses.
Compared with people who took a low dose of 400 IU daily, patients who took high dose vitamin D (4,000 and 10,000 IU) unexpectedly had a greater decline in their bone-mineral density. In some trials, vitamin D supplementation to achieve levels of 28 to 40 ng/mL did slightly lower fracture risk.
Vitamin D3 Supplements do not prevent or improve depression in elderly people, and likely do not help other age groups either.
One trial showed a modest reduction in the incidence of type 2 diabetes, while another showed no benefit.
Supplementation with vitamin D did not result in a lower incidence of invasive cancer than placebo.
So this is why we shouldn’t be screening everyone for vitamin D deficiency, according to the US Preventive Services Task Force, and a lot of other consensus. This includes your average healthy person at a routine annual physical. A lot of insurances no longer cover the test without a good reason, so you might get a bill, too. Instead it’s better to remind people in good health to get enough vitamin D from their diet and some time outdoors. See previous post for more details on how to do this. And here are the Recommended Dietary Allowances (RDA) for vitamin D:
600 IU daily for people from age 1 to 70 years old
For adults 71 years and older, 800 IU daily is recommended for the prevention and treatment of osteoporosis.
Is there much harm in supplementing with vitamin D above and beyond these dietary allowances? The evidence suggests not really. But with too much supplementation, we can sometimes over do it. This leads to high calcium levels, which can cause neurological symptoms, cognitive problems, gastrointestinal issues, and kidney stones.
But if you do have your vitamin D levels checked - either because you are at higher risk for deficiency, or because you just want to know despite the shady evidence of benefit, and are willing to eat the bill for the blood test that might not get covered - this is what some experts recommend doing with the results, and it seems reasonable to me:
Vitamin D levels <12 ng/mL - treat with 50,000 IU orally once per week for 6 to 8 weeks, and then 800 IU daily thereafter.
Levels 12 - 20 ng/mL - supplement initially with 800 to 1000 IU daily.
Levels >20 to 30 ng/mL – consider 600 to 800 international units to maintain levels in the target range. But as noted in all the studies above, this is far from evidence based! Many adults who are getting adequate calcium and vitamin D from dietary intake and sun exposure do not need to take any supplements.
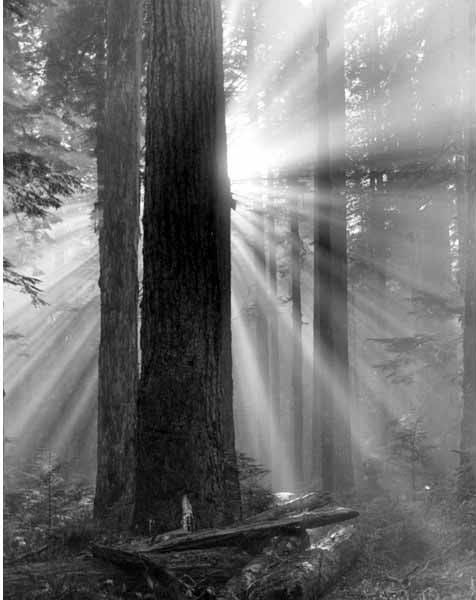
My own take on the paradox between associations of vitamin D with certain illnesses, and the disappointing results we see with vitamin D supplementation is based on two main ideas. First, I think that the many conditions predisposing people to low vitamin D levels also contribute to other medical risks. For example, people with obesity are at higher risk of developing vitamin D deficiency, but also have a higher risk of diabetes because of that obesity. Secondly, I think the timeline matters. Maybe we can’t make up for years, decades, or lifetimes of low vitamin D by taking a supplement in these clinical trials for 1-6 years. Maybe the ounce of prevention being worth a pound of cure really applies here. Primary care advice to be aware of ways to optimize your vitamin D dietary intake and get outdoors a bit more, and to get screened and supplement if you are at higher risk, applied over decades, probably makes a much bigger difference than our narrow time frames of study would pick up. Does that sound reasonable?
And so in conclusion, vitamin D matters, but perhaps not in the ways we think it does. It is a hormone, primarily responsible for regulating calcium in the body. We know it’s important, because with very low levels we see rickets in children and osteoporosis in adults. The evolution of human and Neanderthal skin color and genetics was likely driven by UVB light intensity decreasing as we moved north. There is an undeniable association of multiple medical conditions with low vitamin D levels, but we cannot make a reductionist leap and say this is the only factor in play. If it were, then we would not see such consistent failure of vitamin D supplementation in reversing and preventing these same associated diseases. It makes sense to avoid deficiency by reviewing the good dietary sources of D, and getting outdoors - but not too much - that impossible balance between skin cancer risk and stimulating our own vitamin D factories. Testing and supplementation are most likely to help those at higher risk, including the elderly and those with certain medical problems that limit absorption and production of D. When in doubt, a low dose supplement as mentioned above, especially in the winter, is a low risk and maybe somewhat helpful compromise.
And when all else fails, and you are completely confused, just remember that a diet rich in seal blubber and offall does provide enough dietary vitamin D to compensate for mimimal UVB exposure. Or to quote the New England Journal of Medicine:
…the high frequency of vitamin D screening continues unabated, with frequent requests from patients for screening and advice for supplementation. A reasonable response to low-risk patients is that the National Academy of Medicine's recommended daily allowance for vitamin D is 600 to 800 IU.
Bu there are no simple questions, or answers!
In sunshine and rain,
Ryan





Excellent information. Thanks!
Thank you!