Covid. When I look around I realize I am an outlier to still care. Maybe you are, too. But if we are doing our jobs well in primary care we should still respect this virus. And Covid is definitely on the rise again right now. I had a patient come in last week for a routine physical. He admitted he “had a cold.” It was obviously something. I asked him to put a mask on for other people, including the 101 year old who was in the same waiting room. I recommended we test him for Covid. He obliged. He was very positive +++. We treated him, mostly to reduce his chance of long Covid. He’s doing well. Draw your own lessons. I keep my mask on when seeing people in small examining rooms.
Another one of my patients was admitted to the hospital last week with Covid. She felt horrible, and developed serious heart problems after a previous infection. I shared my self-treatment plan with her, and she discussed it with the Infectious Disease specialist taking care of her. If you’re a primary care doc trying to hang with the ID docs, it boosts your street credibility to cite the sources, and I do.
I was on call this weekend. Received 2 emergency calls about Covid infections. Treated both. One is going for it with metformin to reduce long Covid risk. We will see if he tolerates the GI side effects. Most, but not all, do.
So welcome back to some monthly highlights from a place I call Covidlandia, a forgotten land between black and white, carefree and cautious, pandemic beginning and end. I present recent news, scientific discoveries, and medical knowledge that caught my attention and that is of interest to primary care. I curate and comment, and realize that one human being cannot possibly keep up with everything. But I try to highlight useful, actionable stuff. January, February, March, April, May, and now June.
What’s up with Covid rates right now?
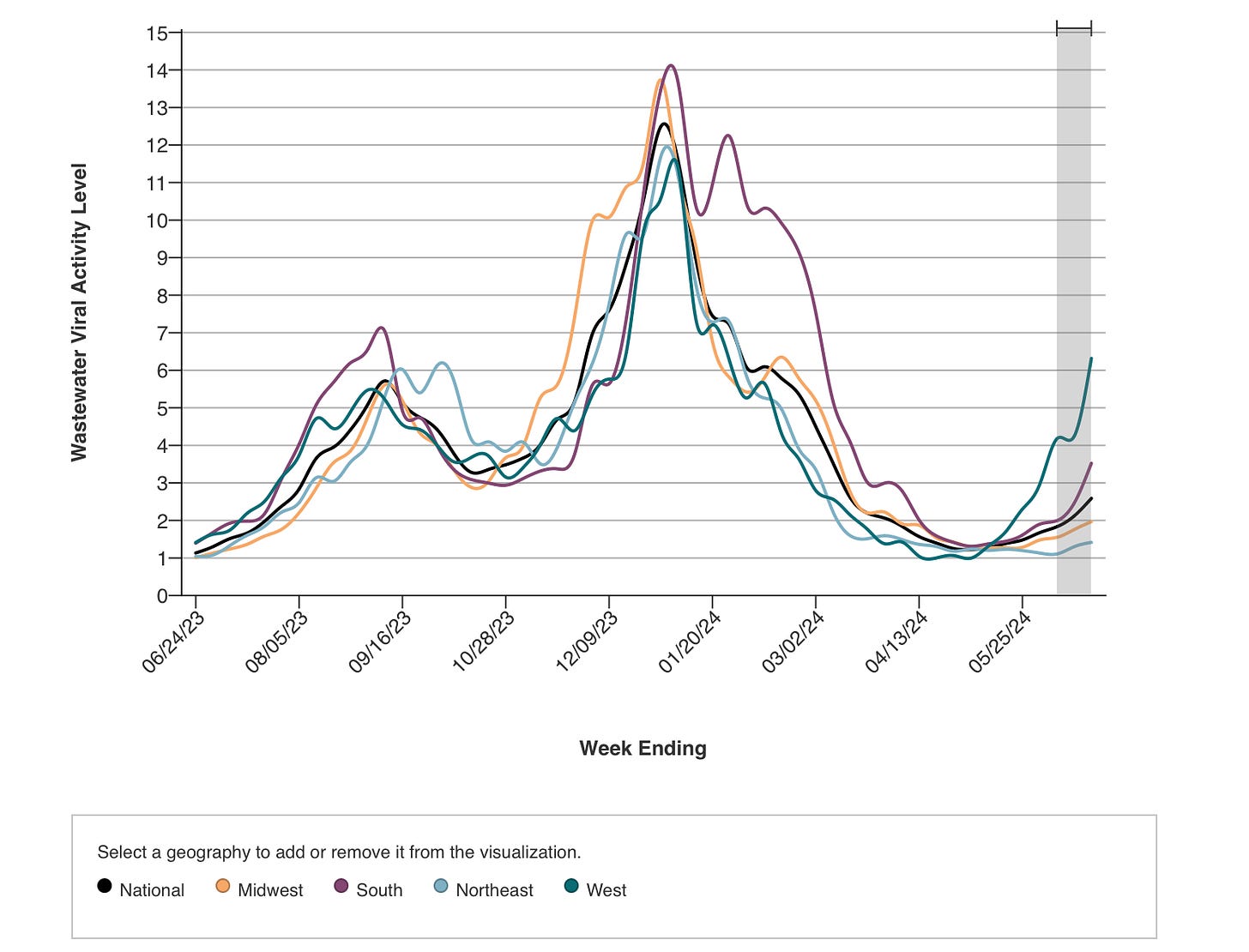
Globally cases are increasing. Here in the U.S. the western and southern states are seeing the sharpest rises, but you can check your local rates by reviewing the sewage analysis trends via CDC Data Tracker or WastewaterSCAN. Pretty much every U.S. state is on the way up.
From the CDC, with data that is about a week old:
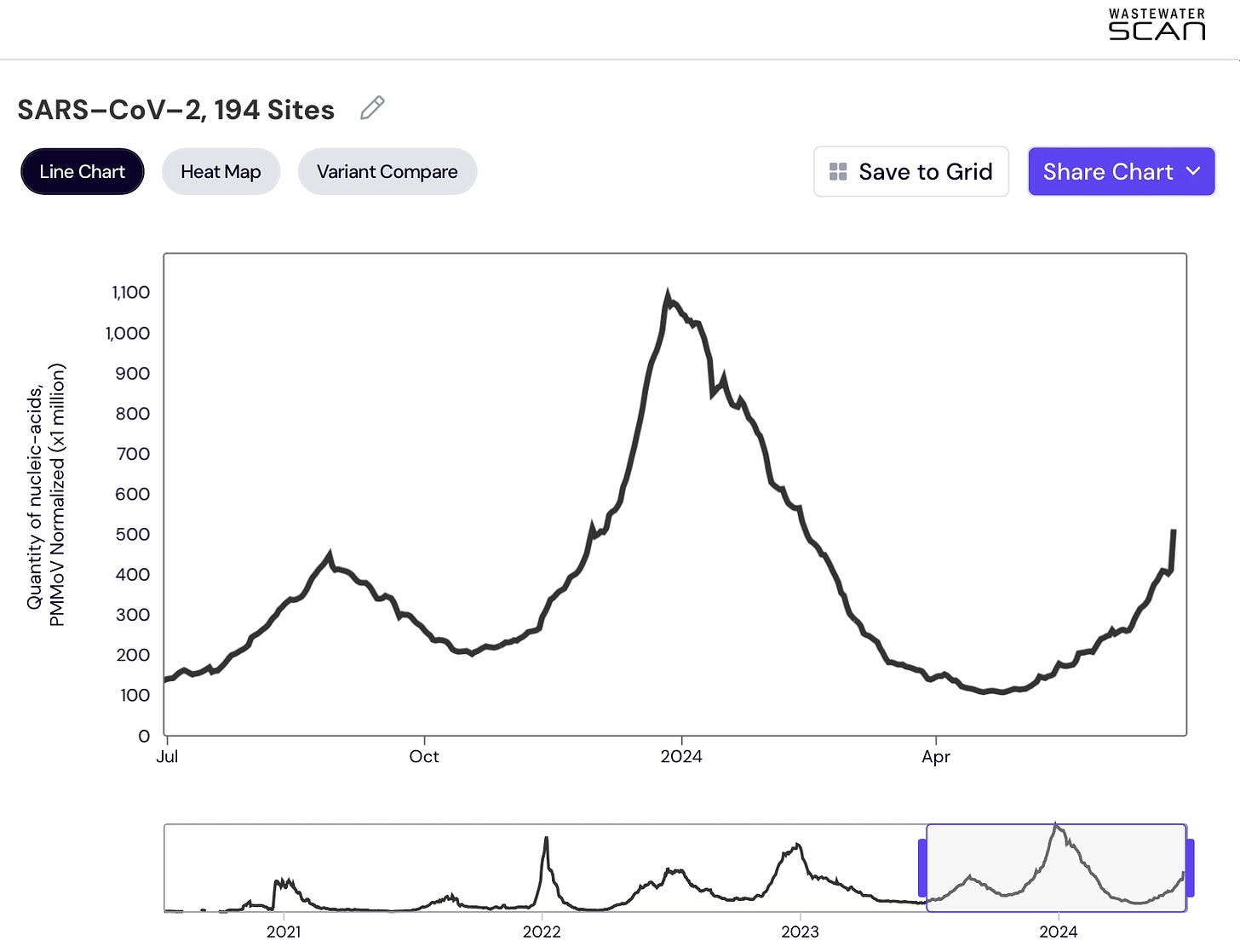
You can clearly see the trends here, unless you are colorblind, in which case few graph-makers really care. I know from personal experience. Nonetheless all the lines are bending upwards. Here is another view of what the national trends look like overall, per WastewaterSCAN, with data a bit more recent than the CDC’s:
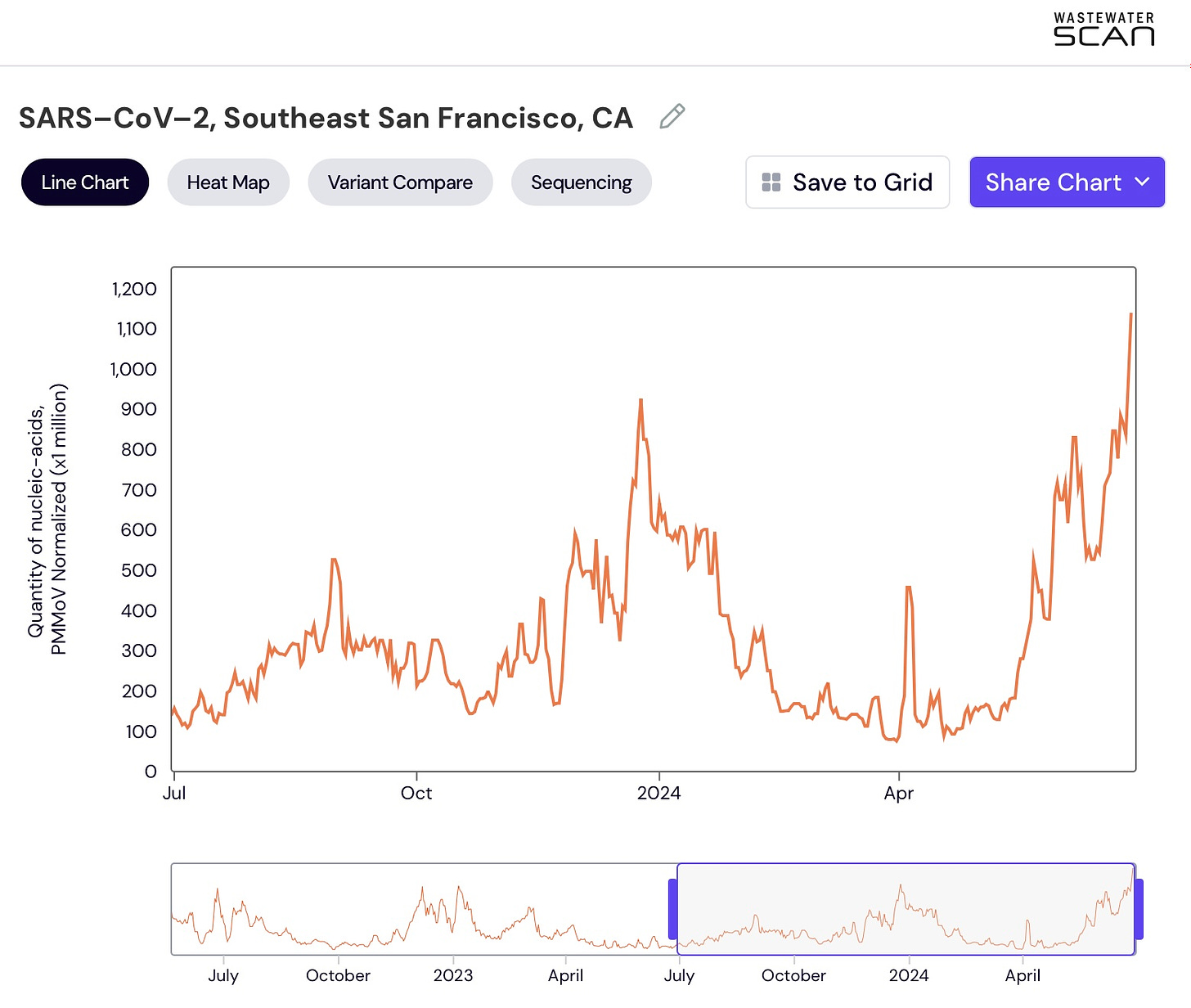
They say as California goes, so goes the rest of the country. Will it be the same with this incipient Covid wave? I think so. Here is data from a treatment plant in San Francisco. SARS CoV-2 detection in wastewater is really high. It looks worse than the holidays to me:
In this treatment plant in San Francisco, 36% of viruses being detected are the KP.2 variant, with JN.1 lineages still hanging around. Nationally the KP.1, .2, and .3 variants make up the vast majority of cases, while LB.1 is steadily increasing. What a depressing horse race to follow.
Compared to late June in previous years, we are not doing great right now:
Compared with 2023, we are at 1.9x higher Covid prevalence now Late June 2022 was actually worse than now, coming in at 2.3x higher (BA.2) than now Compared to 2021, we are 5.6x higher now Compared to 2020, we are 2.8x higher now
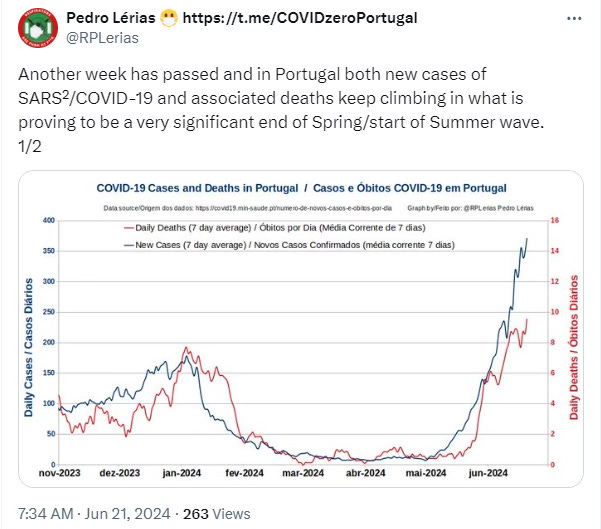
A similar spike is already playing out in places like Portugal. Here is an instructive tweet from a source on the Iberian Peninsula last week (hat tip to Dr. Crystal):
I have no proof that the tasty Portuguese pastry called pasteis de nata helps with Covid. But it is worth the trip by itself. Hang in there, Portugal, and the world.
Personally I have a busy month of July planned, with travel and social stuff. I think there is a decent chance I’ll catch a case. But I’ll try to prioritize ventilation when I can, wear my 3M Aura on the plane, and treat myself according to the plan with an eye on trying to prevent long Covid.
Early use of antivirals linked to reduced risk of long COVID
A meta-analysis of nine observational studies published in the Journal of Infection showed that early use of an oral antiviral drug (like Paxlovid) reduced the risk of long Covid by 24%. Not amazing, but significant. And given the difficulty of diagnosing long Covid without an objective blood test, who knows how much higher that 24% would be if we did check objective markers like endothelial biopsies, before and after CTA scans of the coronary arteries, peripheral nerve biopsies, etc.
An article in CIDRAP about this meta-analysis states:
While antivirals have been approved to use in the acute phase of illness to prevent progression to severe disease in at-risk populations, the potential use of the drugs as a way to prevent long COVID has drawn recent attention.
Really? C’mon. I started writing about this over two years ago. I’ve been following the zeitgeist, not listening to the thought leaders who strayed from the early evidence, and holding firm to my own belief that treating early with antivirals like Paxlovid to reduce viral loads by an order of magnitude should reduce some collateral problems. I even drew a picture of a fruit cake back in March, 2022 to illustrate this. I’ve also been long on using metformin, and that COVID-OUT trial I discussed last month showed a 40-60% reduced risk of long Covid when we are able to stomach the 2 week course of metformin pills.
Statin drugs might help a little in the treatment of Covid
A pooled analysis of very sick patients treated with cholesterol-lowering meds called statins (think rosuvastatin/Crestor, atorvastatin/Lipitor, etc) showed a 12% reduced risk of death by starting a statin while sick in the hospital.
The meta-analysis included 7 randomized controlled trials comprising a total of 4,262 patients. However, the statistical confidence interval was not great [CI], 0.80-0.98, and so the true percentage of mortality risk reduction lies somewhere between 20% and a measly 2%.
But as more guidelines support this, I at least try to keep patients on their existing statins during treatment with Paxlovid, either by reducing their dosage or switching to pravastatin for 5-10 days (as this has minimal interaction with Paxlovid). Statins have beneficial anti-inflammatory and immuno-modulatory effects in atherosclerotic plaque, and now we know that SARS CoV-2 viruses can directly invade coronary arteries.
Antivirals molnupiravir and remdesivir are fine with statins, but confirm that individually with your doc as part of a comprehensive medication review.
N95 masks are still excellent tools for preventing viral transmission
A study published in The Lancet eBioMedicine compared the effectiveness of different types of face coverings in preventing SARS-CoV-2 transmission. Researchers collected breath samples from Covid-infected people wearing various masks and respirators. The results showed that all face coverings blocked/reduced exhaled virus by at least 70%, but the N95 respirators were the most effective, blocking 98% of the viruses.
Interestingly, KN95 masks underperformed cloth masks in this study. I think this is probably a unique quirk of just one study, but the authors did comment that often KN95s are more stiff and don’t conform to the face as well. A well fitting “cloth” mask like an Enro brand might do better than a poorly fitting KN95.
The lead author confirms that N95s win because of their tight seal, powerful filter, and large air space behind the mask. I don’t get on an airplane without one. And politicians in North Carolina, New York, and elsewhere who are legislating mask bans should be stopped. Shamed, really.
Airplanes are vectors for ruining your trip with an infection
Speaking of airplanes, this study is very convincing. In a systematic review performed by researchers at Stanford and CHOP here in Philly:
Researchers analyzed 50 flights from 15 articles published between January 2020 and April 2021. They found that longer flights without masks significantly increased Covid transmission risk. Medium-length flights (3-6 hours) had about 4.7 times more cases than short flights (under 3 hours), while long flights (over 6 hours) had nearly 26 times more cases. Each additional hour of flight time increased the risk by about 1.5 times. Importantly, long flights with enforced masking reported no transmission. Wow.
I’ve been up and down in a plane about 16 times since this started. I’ve worn an N95 each time. Viruses including SARS CoV-2 are currently 0 for 16 in that timeframe, whereas I probably got sick with something on half of my previous trips before the pandemic.
More than 200 symptoms tied to long Covid
A ground-breaking report from the National Academies of Sciences, Engineering, and Medicine presented conclusions about long-Covid diagnosis, symptoms, and impact on daily function. They list over 200 potential symptoms, which makes it quite an umbrella diagnosis and further complicates any easy way to deal with this in primary care.
The report found that 5.3% of U.S. adults (13.7 million people) currently have long Covid as of April 2024, with women nearly twice as likely to be affected. The chance of developing long Covid, at least temporarily for months, ranges from 10-30% after infection, depending on which study you look at.
While most people improve over time, recovery can plateau at 6-12 months, and only 22% fully recover by one year post-infection. The condition poses challenges for disability benefit systems, as its varied and evolving nature makes it difficult to map onto existing eligibility criteria.
Among the 200 possible ones, the key symptoms of chronic fatigue, cognitive impairment, and autonomic dysfunction can significantly impair daily functioning but may not fit neatly into existing disability categories.
These numbers seem high to me, but really disturbing nonetheless:
87% of long Covid patients have some degree of post-exertional malaise (PEM). PEM means that even minor physical or mental activity can reduce a person’s energy and cause a worsening of symptoms in subsequent days.
24% of people with long Covid have some degree of cognitive dysfunction, manifest as some combination of trouble with thinking, memory, attention, processing information quickly, language, and executive functions like problem-solving or multitasking.
At least 25% to 66% of people with long Covid have autonomic dysfunction which can include POTS (postural orthostatic tachycardia syndrome). Symptoms can include elevated heart rate, imbalance, lightheadedness, nausea, and trouble being upright/standing for long.
40 – 70% of long Covid patients meet criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome, and 39% for fibromyalgia.
CIDRAP, STAT News, and National Academies as sources.
I have some good friends and plenty of patients going through this. We are learning more about treatments, but for now it’s still a slog for many. We should try to reduce the number of Covid illnesses we sustain when possible, stay up to date with recommended vaccines, take antivirals when sick, and be compassionate with ourselves if some of this does set in. We are all just trying to live our lives in incredibly challenging times, on multiple fronts.
And people are not freaks when they want to protect themselves. Gaslighting, Covid-trivializing doctors, however, don’t deserve our attention. It pains me that some of them have wide audiences, even here on Substack.
More thought leaders cast shade on Paxlovid
Maybe you heard about a study published this month showing that Paxlovid doesn’t work for those hospitalized with “Covid pneumonia.” Words like “flop” and “hefty blow?” I really don’t understand why some seize on every niche study of Paxlovid that doesn't show that niche benefit, and then extrapolate to common situations and proclaim nails in the coffin for the antiviral medication in general. Or that prescribing antivirals is only for reducing hospitalization and death. Maybe for some ER doctors this is what it is all about, but I live in primary care. And we are swimming in the subtle, cumulative, collateral damage of Covid with many of our patients.
So without getting lost in the weeds of a hot mess of a study, which is quite irrelevant to primary care, I’ll simply quote an astute physician commenter who points out:
Paxlovid was not approved for treatment of COVID pneumonia. The current understanding of the mechanism of Paxlovid is as follows:
Paxlovid was supposed to be given in the viral replication (early) phase of COVID infection to reduce viral load.
By the time the patient is hospitalized, they are in the inflammatory phase and Paxlovid is not expected to be effective.
Therefore, that Paxlovid is found to be ineffective in patients hospitalized for COVID pneumonia, while disappointing, is not unexpected. No big news to get excited or distressed about.
I’ll add that the patients in this study were hospitalized and already on steroids, which means their doctors classified them as being critically ill, severely ill, or having low blood oxygen levels. Many of them were also on other antivirals and monoclonal antibody treatments. But when crappy preprint studies get major platforms, you get lots of other commenters saying stuff like this:
No one is pushed forward since the evidence came out about ivermectin being a better choice. It's interesting how many studies were squelched knowing that there was positive evidence. The medical community is sold out.
or this:
The drug simply doesn't work. Additionally, the drug was never effective for anything other than make $$$ for the pharmaceutical company.
Ugh.
And ironically there was another study last month that showed the opposite result. Severely ill, hospitalized patients were found to do better when given Paxlovid even after the 5 day window since symptom onset had elapsed. Granted this was a cohort study, so not definitive proof. But we already have evidence that another antiviral (remdesivir) can help when given to hospitalized patients, even out to 10 days after symptom onset per guidelines.
I reserve the right to correct myself if indeed better studies show Paxlovid and other antivirals don’t have a place at the primary care table. But as of today they still do, and the ID Society of America guidelines and NIH guidelines are well-referenced and authoritative.
Paxlovid not a panacea for treating long Covid
In people suffering from long Covid already, I’ve occasionally tried using Paxlovid to potentially clear out pockets of lingering virus that have been seen in a small subset of this umbrella condition. The NIH and others are actively studying this, too. It has worked miraculously in a few, maybe 20%, and ho hum in others. Anecdote here.
A recent study found no benefit from taking 15 days of Paxlovid in patients who have well-established long Covid. But once again, this does not mean all-or-nothing. Problems with this study include that these patients had already been suffering from symptoms for an average of 17 months. Perhaps earlier treatment would have helped a statistically significant proportion. They only studied 155 people, so a subgroup analysis would be very difficult.
Nonetheless I’m sad about this, as I’m sure millions of other people are, too.
Fall Covid vaccines being cooked up as we speak
The CDC's Advisory Committee on Immunization Practices (ACIP) this month recommended updated Covid vaccines for the upcoming fall/winter season.
In a unanimous 11-0 vote, the ACIP recommended that everyone 6 months of age and older should receive an updated Covid-19 vaccine, same as last year's recommendation.
Moderna and Pfizer mRNA vaccine manufacturing will be nimble enough to target the KP.2 variant, while word on the street is that slower Novavax manufacturing has already begun and is targeting the older JN.1 variant. Both vaccines will likely help reduce infections for months, and severe disease/death durably. Protection against severe disease is incremental at this point, especially for the young and healthy, since almost everyone has some combination of prior infections and vaccinations. But the older we get, the more important these updated vaccines become against severe disease. For the younger crowd: less infections + milder infections = less long Covid + sick family members.
Take home
Covid rates are going up in the U.S., and have been high in other parts of the world for a while now.
Early antivirals reduce the risk of long Covid. We are still seeing evidence of this.
Starting a statin medication in hospitalized patients with Covid might help a little, but the evidence is not compelling. More intuitively, staying on a statin with immunomodulatory effects while sick with Covid, and a virus proven to infect the vascular endothelium and indeed atherosclerotic plaque itself, makes sense. Talk to your doctor about specifics.
N95s work.
Airplanes are speeding rockets full of coughing people, and N95s work. Being sick with anything on vacation sucks.
Long Covid is formally recognized as having 200+ possible symptoms, but with core ones like post-exertional malaise, brain fog, and autonomic dysfunction leading the way. Don’t let the counter-narratives fool you.
Paxlovid is still an effective tool, especially in outpatient primary care, unless better studies prove otherwise and cancel the quality evidence the Infectious Disease Society of America and the National Institutes of Health have based their treatment guidelines upon. If you’re going to come at the kings, you best be ready.
Granted, 15 days of Paxlovid disappoints in a small study of 155 people with long Covid for an average of 17.5 months’ duration.
I’m staying up to date with Covid vaccines, and will happily roll up my sleeve in the fall for one.
Take good care!
P.S. My daughter and I were watching a NOVA episode last night about artificial intelligence, and we decided to have a chat with Claude.ai. She asked this AI chatbot to write back to her “like a cool teenager” would. Funny dialogue. I then went one step further and copy and pasted my June Covidlandia conclusion above, and asked it to rewrite it as a cool teenager might… here’s what we got! Is this more effective health and science communication?
~
🤖
Alright, check it out, fam. I'm gonna give this COVID talk a fresh spin:
Yo, listen up! COVID's making a comeback in the States, and it's been wildin' out globally for a minute.
Here's the 411:
- Snag those early antivirals and you might dodge the long COVID bullet. Facts!
- Statins for hospital patients? Meh, jury's still out. But if you're already on 'em, stick with it. Your doc knows best.
- N95 masks? They're the real MVPs. Don't sleep on 'em.
- Planes are like germ party buses in the sky. Mask up or risk catching whatever's going around. Vacay sickness? Hard pass.
Long COVID's no joke - it's got more symptoms than a hypochondriac's diary. Don't let the haters tell you different.
Paxlovid's still in the game, holding its own. Unless some next-level research comes through, it's the go-to for now. Don't mess with the big dogs at IDSA and NIH without solid proof.
But heads up - Paxlovid ain't doing much for the long-haulers. Bummer.
Your boy's staying current with those COVID shots. Catch me in the fall, sleeve rolled up, ready for that new-new vaccine. Stay safe, stay smart!
🤖
~
🙋♂️
A sincere thanks as always to upgraded subscribers. If you like these updates and the rest of the work that goes into writing Examined, upgrade your subscription, and then join us already for the afterparty in the comment salon :}
Happy 4th of July in America 🇺🇸
Freedom. Liberty. Independence. Can you imagine them outlawing a public health tool and personal protection choice like wearing a mask when we choose to?
Before we ban AK-47 assault rifles?















I sure wish we had head to head trials of mRNA vaccines vs novavax: the Moderna RSV vaccine has dismal protection after a few months and I’d like to know if waning immunity is due to the platform— some extremely important decisions are looming for the fall, and which COVID vaccine to get is one of them.
Thank you so much for this update! As someone who has been very very careful, I’ve loosened up and there is a strong urge to throw caution to the wind and be like everyone else. But, realistically, I’m at higher risk and don’t want to be sick.
Recent bizarre moment: I’m masked in my Harvard hospital primary immunodeficiency clinic, explaining to the unmasked immunologist that I mask in medical facilities and public transportation as he says “good plan.” Crazy right? All the patients are immune compromised…
This just came into my inbox, so I thought I’d give a little shoutout to the Village Apothecary, which is also validating what Dr. McCormick has written here about the current Covid numbers. The Apothecary head pharmacist writes:
We're the Hudson Valley's Best!
First, a big thanks to you all for voting for us in Chronogram's 5th Annual Chronogrammies.
Village Apothecary won for Pharmacy. I won for Public Health Advocate/Activist! What an honor for me and the team!!!!
I appreciate how you all feel and I will keep up the good work to be deserving of this recognition...
...like keeping you updated on vaccines :)
Your Summer Update - COVID Surge!
If you're even half paying attention, I hope you've seen that COVID is surging once again.
This should not be a surprise to anyone; nearly every June/July since this thing started we've seen a run up of infections as the Omicron strains keep mutating.
We expect a small reprieve at the end of August, followed by the beginning of our big fall surge.
Here's your vaccine update to get you oriented to the current situation and prep you for the fall [there is lots more, but this gives the idea—this little independent pharmacy in Woodstock, NY, was a savior for a lot of us, particularly when vaccines were scarce—they did community outpost vaxing, as well as onsite, and he, like Dr. McCormick and Dr. Jetelina, work hard on public-facing communications].