You are finally being seeing by your primary care doctor. You had to wait a long time just to get an appointment. He’s running late. The front desk asked you a bunch of tedious questions. That double latte you drank in the waiting room now has your heart pounding, and you have to urinate. Badly. A medical assistant brings you back quickly. They ask you to climb up and sit on an examining table that feels much too highly perched. You make some small talk about how crazy the traffic was today as they quickly take your blood pressure through your shirt sleeve. 159 over 93. What? you exclaim. It’s been much better at home! The doctor barges in, and before you know it he’s prescribing your third blood pressure medication. He’s leaving the room already. What’s happening?!
Among the many problems with our healthcare system is the challenge of getting a proper, accurate, efficient, and consistent blood pressure reading in clinical situations. As one of the core vital signs we measure in the office, ER, and hospital, you would think that clinicians and patients would know the basics of how to do it right.
And so here is the next installment in my quick boost series - the vital and overlooked foundations of a good blood pressure assessment.
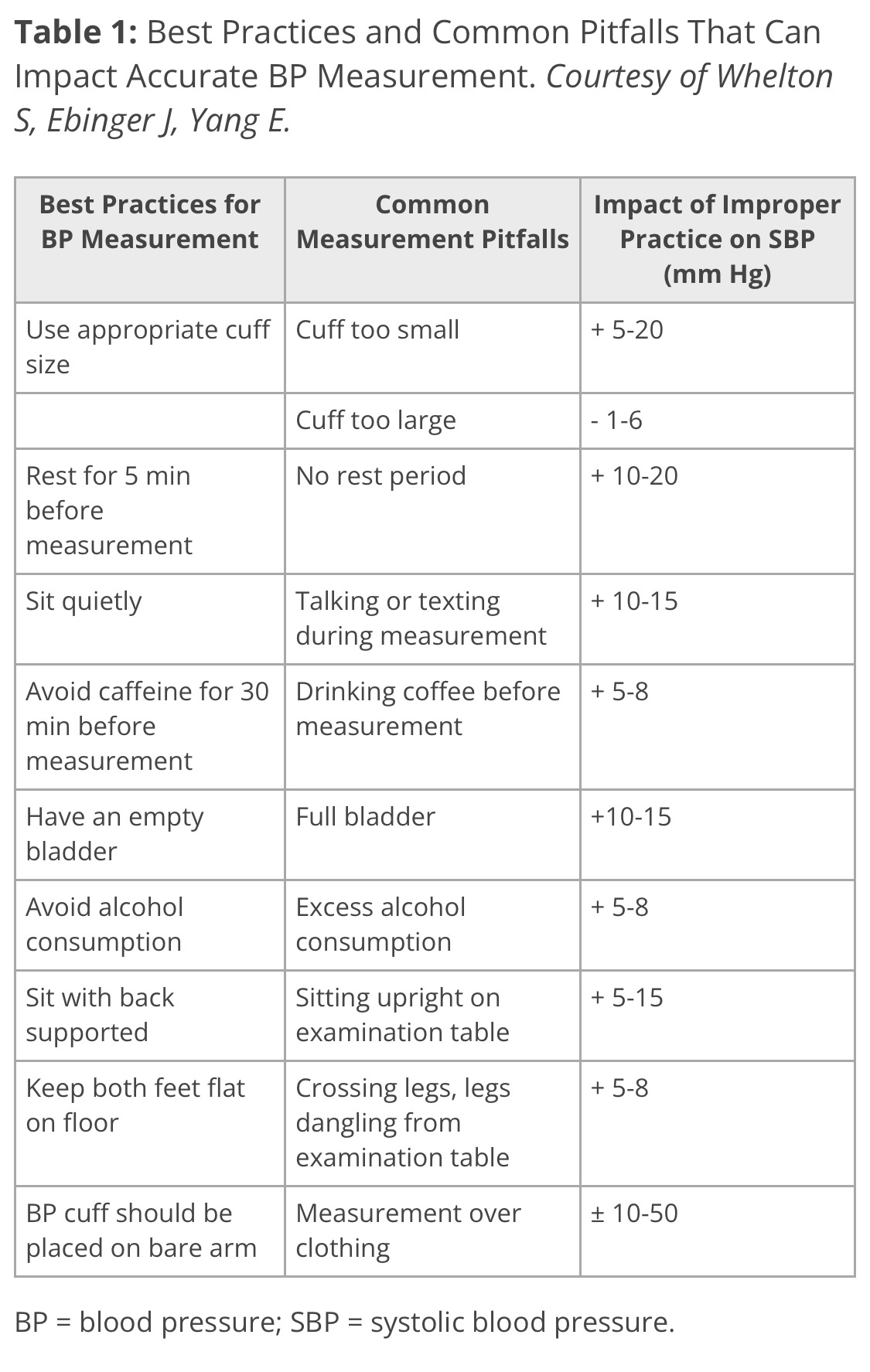
Nine of the most common problems adversely affecting a good blood pressure measurement were cited in an article published by the American College of Cardiology. The degree by which each factor can overestimate our actual blood pressure ranges from a little to a lot. If we add them all up in a worst case scenario, we might panic that our blood pressure readings are actually up to 100 points too high! This is obviously not the case except in very rare circumstances. But it’s still important to know these, and to do our best chipping away at sloppy techniques. Those nine:
☑️ Use a proper cuff size. Cuffs that are too small for a person’s arm can give artificially high readings. With very large arms and small cuffs, up to 20 extra points of inaccuracy was recently demonstrated in a study published in JAMA.
☑️ Rest for 5 minutes before measurement. This is logistically difficult in primary care settings where we have about 20 minutes per patient visit, loaded as each can be with 20 unique problems at times. I often try to double check a high blood pressure when I first walk into the room.
☑️ Chill quietly during the measurement. If you’re going to measure, measure. Don’t talk. Or text.
☑️ Avoid coffee and caffeine for 30 minutes. Everyone can experience a quick jolt in blood pressure right after drinking coffee. This effect is mild in people used to drinking coffee. It is more pronounced in people who don’t usually drink coffee. Overall drinking coffee is safe, unless you have very high blood pressure.
☑️ Empty your bladder. We have all experienced a full bladder and the discomfort that goes along with it. It turns out that this bladder distention activates the sympathetic nervous system and can lead to quite a significant rise in our blood pressures.
☑️ Avoid alcohol consumption. After holidays and weekends I note blood pressures that are worse than usual for many reasons. Much to my chagrin, the less booze we drink the better. I wrote previously about the pleasure and poison of alcohol.
☑️ Sit with your back supported. Core muscles firing and bad posture can mess up a good reading. Most examining tables can be converted so that our backs are supported, or we should sit back in our chairs. The arm should also be supported at the level of the right atrium (mid-chest).
☑️ Keep both feet flat on the floor. This can be difficult when legs are dangling from the high altitude examining tables found in most offices. For many people it takes constant focus not to habitually cross one’s legs. In general this impedes good venous blood flow, too, and can accelerate varicose veins and worsen edema.
☑️ Place the BP cuff on a bare arm. Several sources I read quoted this same wild range of variation, with up to 50 points systolic overestimation occurring! I doubt such a massive increase is common. But one of my sage 95 year old patients tells me each time she visits that she “is wearing her doctor blouse today.” Said blouse allows for easy and expert exposure of the bare upper arm, and I credit her with prioritizing this better than I do.
~
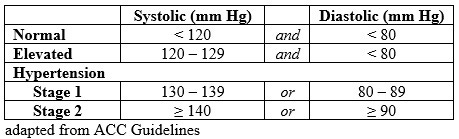
A quick reminder that ideal blood pressures are lower than we might know or hope!
Let’s try to work together as clinicians and patients to check as many of these boxes as possible during blood pressure readings in clinical situations and while doing home blood pressure monitoring.
Increasingly I value the measurements people get at home more than the performative, stressful acts we read like tea leaves in the office. Telemedicine for monitoring hypertension might sound like a bad idea at first, but once the accuracy of someone’s monitor has been assured against a reading performed in the office, and they master the techniques above, checking off all these boxes is certainly easier from home in some ways.
And finally a big welcome to all the new subscribers this past week! Stop by the Examined website for more dialogue after each post, the reading room to catch up on what you’ve missed, and the quick boost homepage for other short and sweet posts. But please beware of the studious cat that shows up sometimes unexpectedly, especially if you have allergies like me.
Take good care.





Omg this is so interesting and helpful!
I’m going to practice these checkboxes to keep my BP lower, whether in the process of measurement or not. The full bladder / sympathetic nervous system activation really “feels” true. Probably important to urinate when nature calls for several good reasons - BP, UTI prevention, continence preservation, etc.
There you go, an idea for a future post ✌️
Great information! I have, as of late, noticed my primary care physician’s staff using a manual bp cuff vs the machine. I mentioned that to the med tech and was informed that my doctor herself made that change due to inaccurate readings. In my bedside nursing days, I’ve always preferred to recheck BPs manually.
I worked a short stint in a “BP check clinic” years ago and learned to make sure my patients always kept feet flat, stop talking, correct cuff size, take a few deep breaths and arm chest high.
As always, thanks for the good work and information!
Happy New Year!