Measles vaccine considerations during the current outbreak *examined*
The deep dive version!
Yesterday I got a lot of questions in real time from patients about whether they should get an MMR booster to shore up their defenses against measles. I sent a quick boost answer based entirely on CDC guidance, and hopefully this was helpful. But I want to dig deeper. So after seeing patients and getting home, I crunched through some stuff until 2 AM, and then cleaned it up this morning. I hope you also find this helpful. It is sourced from over 100 citations and I had to leverage Perplexity to help me synthesize it.
Please consider this as educational information, and then make your own decision in consultation with your doctor if needed. Me? What am I doing right now as a healthcare provider in a measles outbreak that has reached my backyard in Jersey? I checked my dusty vaccine records. Looks like I got 2 MMR shots as a little kid. I then had a 3rd shot in 1991 which I don’t remember. Turns out there was a measles outbreak in Philly that year. Over 1,400 people (mostly children) became sick with measles, and nine children died. The epicenters were unvaccinated children in fundamentalist churches that relied on faith healing. Crazy I don’t remember this, though I do remember Operation Desert Storm that expelled Saddam Hussein’s Iraqi invasion of Kuwait that year. My astute family doctor must have given me that third shot. I’ve had MMR blood titers checked during med school, and then again when starting my practice as an attending. I had protective antibodies. That was 20 years ago, so I’m tempted to check them again… but guidelines might suggest this is excessive.
If I’m told by public health leaders or other trusted sources to roll my sleeve up for another shot now, I absolutely will. And if we start hearing about mumps I will get another MMR, too.
So what about you? What does the CDC consider adequate protection in general, and during times of measles outbreaks? As long as you have presumptive evidence of immunity they state you are ok right now.
Acceptable presumptive evidence of immunity to measles includes:
• Written documentation of adequate vaccination
• Laboratory evidence of immunity
• Birth before 1957
• Laboratory confirmation of disease
What is adequate vaccination? Why is this so confusing?
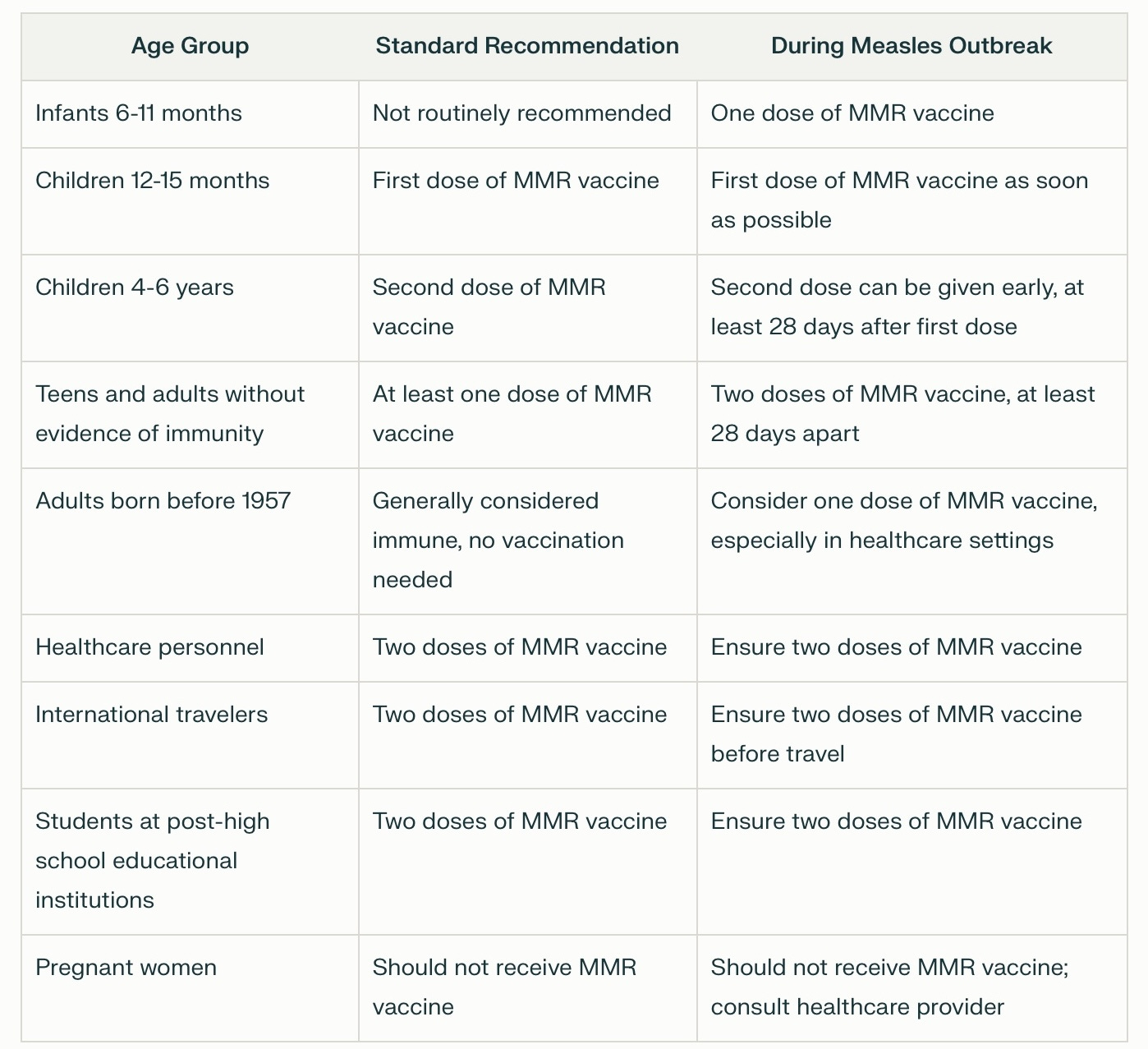
Hopefully this table will help. I made it from CDC guidance. The columns include standard and measles outbreak recommendations:
Notes: During an outbreak, public health authorities may recommend additional doses or accelerated vaccination schedules for certain groups at increased risk. I’ll be watching for this. For adults born before 1957, while they are generally considered immune, during outbreaks or in healthcare settings, vaccination may still be recommended as an extra precaution. If you were vaccinated between 1968 and 1989, you likely received just one dose of the measles vaccine, instead of the two doses that are standard today. Those who only received the killed measles vaccine (1963-1967) should be revaccinated with the current live vaccine.
You can follow the measles outbreak numbers in the US via this CDC resource. Hopefully it will not be censored and manipulated.
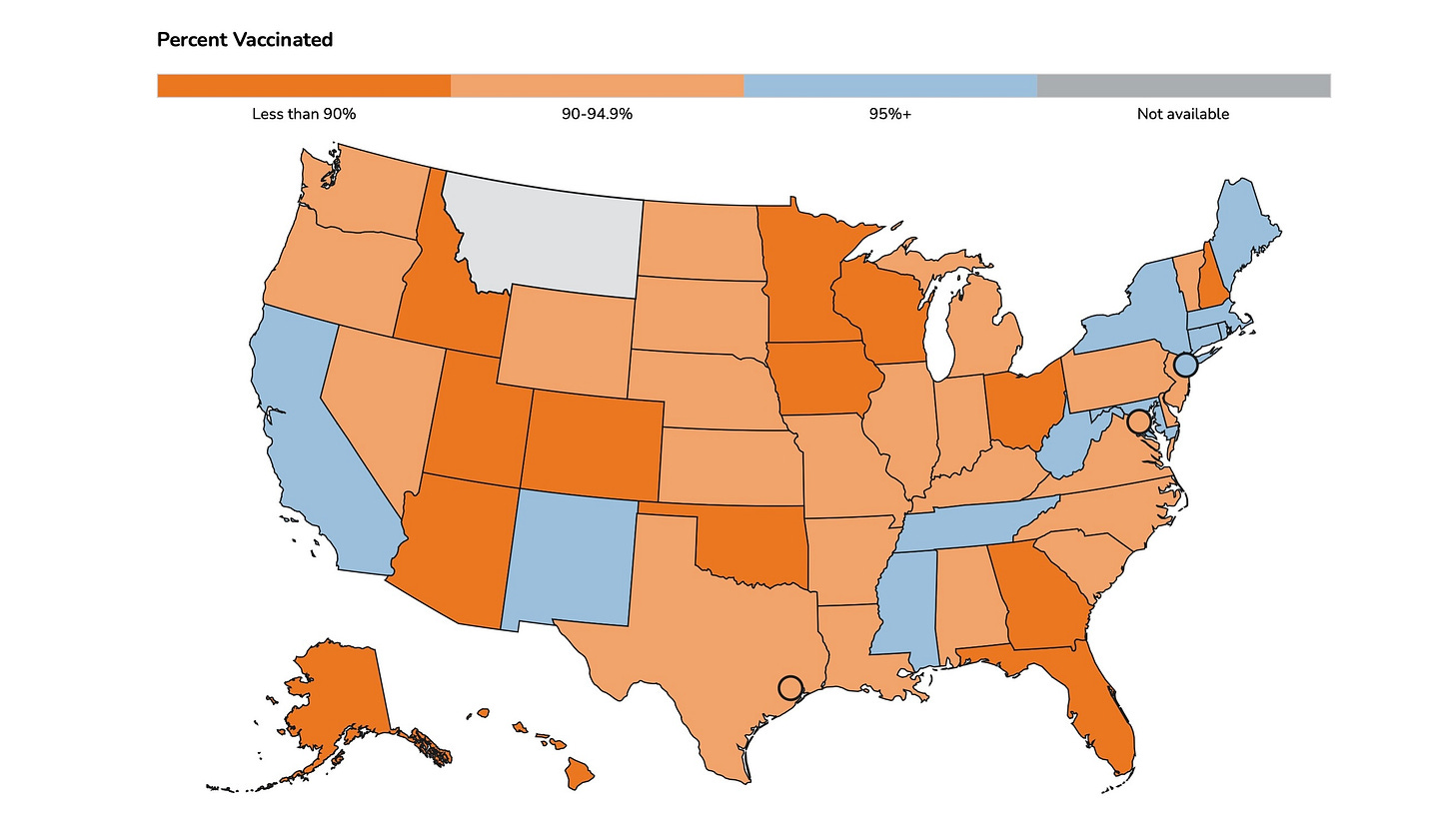
We are not looking good as a country right now in so many ways. Science tells us that at least a 95% measles vaccination rate is needed to keep outbreaks from spreading. How are we doing on that?
You can stop right here if you want. It’s all you really need to know right now. But I had many more questions as a doc, and so I dove deep. Read on if you’re down with that, too. Warning: it is really technical and not written for a general audience, but rather for highly motivated spelunkers.
Recent measles outbreaks, particularly this 2025 resurgence in Texas with over 90 cases so far, have reignited debates about the durability of vaccine-induced immunity and the necessity of adult booster doses. While measles was declared eliminated in the U.S. in 2000, declining vaccination rates and global travel have facilitated its return. The following examines the evidence for and against administering measles boosters to adults during outbreaks, focusing on waning immunity, outbreak dynamics, and public health guidelines.
The Case FOR Adult Measles Booster Vaccinations
Evidence of Waning Vaccine-Induced Immunity
Longitudinal studies demonstrate measurable declines in measles-specific antibody levels over time after vaccination. A 2023 Slovak Republic seroprevalence study found that antibody titers wane at an average rate of 9.7% per year following the first MMR dose and 4.8% annually after the second dose. Now this is just referring to quantitative antibody levels, not disease protection. But by age 33, individuals vaccinated with two childhood doses had geometric mean titers of antibodies (GMT) of 1,331 mIU/mL—a 49% reduction from peak post-vaccination levels. While these titers remain above the protective threshold (≥120 mIU/mL), borderline seronegativity increases with time. For example, 15% of vaccinated healthcare workers in a 2021 study lacked protective IgG levels, compared to 6% of those with prior measles infection.
Even Deeper Dive into Evidence of Waning Vaccine-Induced Immunity
Recent multinational studies reveal nuanced patterns of antibody decline and vaccine effectiveness reduction over time, particularly in measles-eliminated regions. A 2024 Lancet Public Health modeling analysis of England’s 2010–2019 measles cases found that scenarios incorporating 0.04% annual waning of MMR vaccine effectiveness best matched observed outbreak dynamics. This gradual decline becomes epidemiologically significant in elimination settings (lacking natural immune boosting from persistent measles circulating), where 35-year-old adults vaccinated in childhood showed a 12% cumulative reduction in protection compared to endemic regions. The model further estimated that transmission risk from vaccinated individuals (who are supposedly less contagious when sick) still reached 83% of the transmission risk from unvaccinated cases after 30 years, creating susceptibility clusters despite high baseline coverage. Vaccinated individuals who still pick up a breakthrough case are still more contagious than we would like or are being told perhaps.
Antibody kinetics studies complement these population-level findings. A 2020 longitudinal analysis comparing measles IgG levels after two (MMR2) and three (MMR3) vaccine doses demonstrated that measles antibody concentrations reverted to pre-booster baselines within one year of MMR2 administration, yet still remained above seroprotective thresholds. While rubella and mumps antibodies showed slower decay rates, measles-specific immunity exhibited the steepest initial decline—a 1.3-fold reduction from peak titers within 12 months. This aligns with a 2020 meta-analysis of 62 studies showing measles seroprotection rates decreased by 1.2% annually in highly vaccinated elimination settings versus 0.3% in endemic areas where measles is not totally eradicated, with modeled protection dropping below 90% after 25 years in the absence of natural boosting.
High-risk populations exhibit accelerated immune erosion. A 2021 JAMA study of 959 cancer patients found 25% lacked protective measles antibodies, with seroprevalence plummeting to 46% among bone marrow transplant recipients. This waning correlated strongly with time since vaccination: patients aged 30–59 years—who likely received childhood MMR rather than natural infection—had 44% lower seropositivity than those born before 1957. Immunocompromised individuals also demonstrated 2.9× faster antibody decay rates compared to healthy controls in studies, suggesting accelerated immune memory loss.
The clinical relevance of these immunological changes emerges in outbreak analyses. During this current Texas 2025 resurgence, genomic surveillance has identified 17% of cases occurring in individuals with documented MMR vaccination, disproportionately clustered in adults aged 25–40 years—a cohort vaccinated during early two-dose adoption (1989–1995). Attack rates in this group exceeded model predictions based on constant vaccine efficacy, supporting real-world immune decline. Paradoxically, a 2024 U.S. serosurvey found 89% of adults retained measles antibody titers ≥120 mIU/mL, but identified threshold-dependent neutralization deficits: sera from vaccinated adults with “low-positive” titers (120–500 mIU/mL) neutralized contemporary measles strains 3.7× less effectively than high-titer samples.
These findings underscore the interplay between individual immune trajectories and population-level transmission dynamics. While two MMR doses provide durable clinical protection for most, measurable biological erosion—particularly in areas of the world where measles has been mostly eliminated —creates vulnerability windows that facilitate outbreak propagation among subpopulations with waning immunity.
Outbreak Vulnerability in Suboptimally Vaccinated Adults
One more look at the present outbreak as of today. The Texas cases highlight gaps in adult immunity. Among the 58 confirmed cases in February 2025, five occurred in individuals claiming prior vaccination. While incomplete documentation complicates interpretation, this aligns with models predicting 3–5% primary vaccine failure and 0.5–1% annual waning in two-dose recipients. In elimination settings without natural immune boosting, even fully vaccinated populations may develop susceptibility clusters. A 2020 meta-analysis found vaccine efficacy declined by 0.25% per year in such regions, contrasting with stable efficacy in endemic measles areas.
The Case AGAINST Routine Adult Measles Boosters
Durability of Clinical Protection
Despite antibody declines, two MMR doses provide 93–97% lifelong clinical protection against symptomatic measles. It should be reemphasized that waning antibody titers do not equate to lost immunity—immune memory cells persist and mount rapid responses upon re-exposure. Outbreak data support this: in the 2019 U.S. epidemic, 73% of cases occurred in unvaccinated individuals, with only 3% in two-dose recipients.
Natural Immunity Superiority
We have to give it up that hard-earned immunity to measles before the MMR vaccines came along is more durable. But as a preemptive strike against anti-vaccination folks ready to latch onto this truth, consider the terrible price we would have to pay for a bit more durable immunity: nearly 94 million of the estimated 154 million lives saved by vaccines since 1974 were a result of protection by measles vaccines.
Nonetheless, adults born before 1957 likely acquired lifelong immunity through measles infection, which induces higher antibody levels (GMT 213.3 vs. 92.2 in vaccinated cohorts) and lower seronegativity rates (6% vs. 20%). Boosting this group may offer less compelling protection, see table above.
Logistical and Economic Barriers
Implementing widespread adult boosters poses challenges:
Documentation gaps: 42% of U.S. adults lack accessible vaccination records, complicating targeted campaigns.
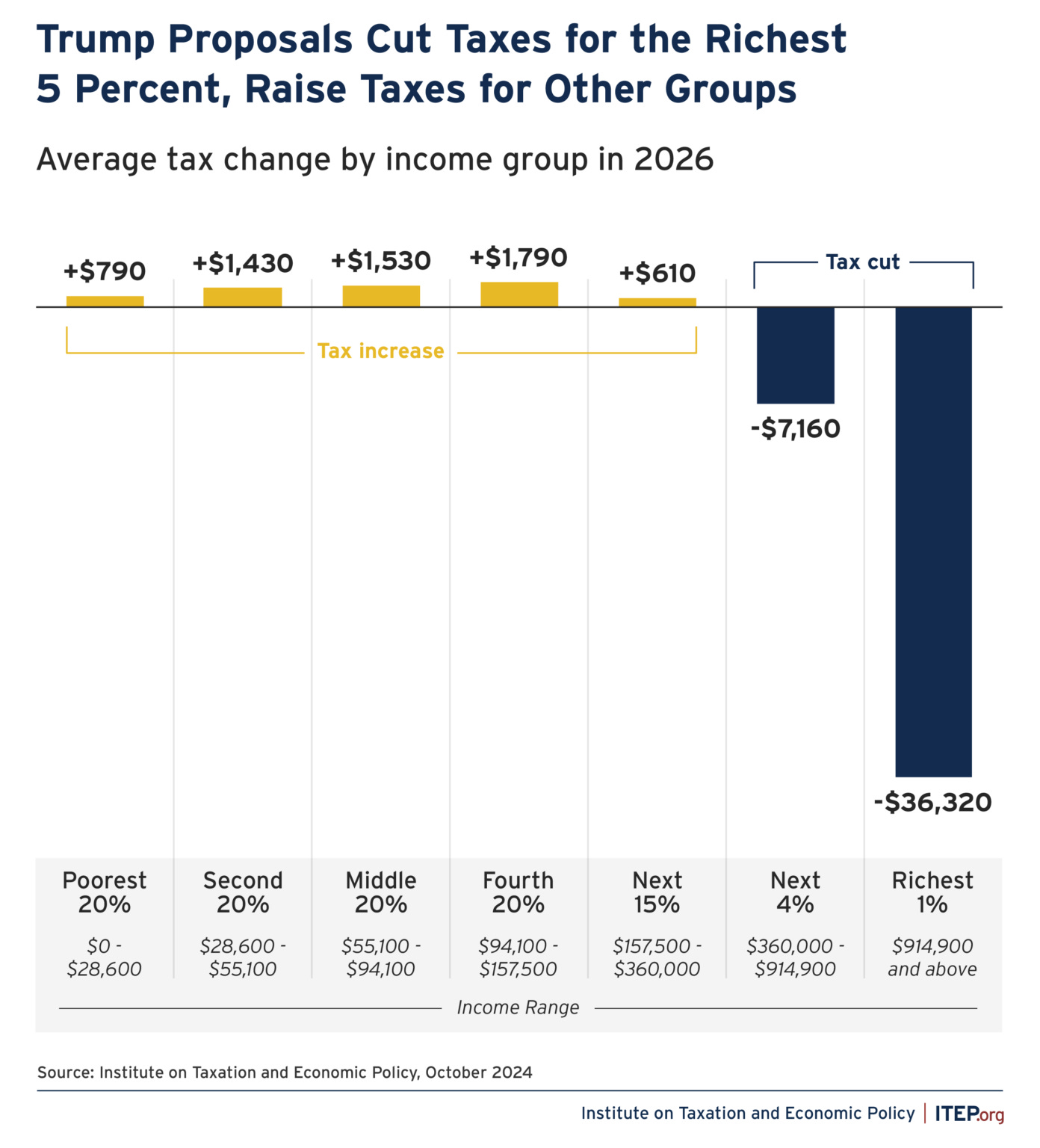
Cost-effectiveness: At $70 per MMR dose, universal boosting would cost $18 billion to cover 260 million U.S. adults—a prohibitive expense given the low attack rate in vaccinated populations. More importantly, we also need to make sure the richest 1% among us receive the lion’s share of the $4.7 trillion dollar tax cuts just passed by the House:
Vaccine hesitancy: Promoting boosters could inadvertently fuel mistrust by implying childhood vaccination is insufficient.
Real-World Outbreak Analyses Revisited
2025 Texas Outbreak Dynamics
The Northwest Texas cluster originated in an undervaccinated community (62% MMR coverage vs. 91% statewide), with secondary spread to five vaccinated individuals. Genomic sequencing revealed this as a B3 strain imported from Europe, where measles resurged due to COVID-19-related pediatric immunization delays. Notably, no fully vaccinated two-dose recipients required hospitalization, supporting vaccine effectiveness against severe outcomes.
Historical Precedents
2015 Disneyland Outbreak: 125 cases included seven two-dose vaccinees, but all had mild courses without complications.
2019 New York Epidemic: 649 cases predominantly affected unvaccinated Orthodox Jewish communities, with attack rates 35× higher than vaccinated neighborhoods.
Consensus Guidelines and Recommendations
Let’s bring this in for a landing by going back to the basics I wrote about in the first couple paragraphs.
The CDC does not endorse routine adult boosters but advises that:
Two documented MMR doses = lifelong protection for most.
Uncertain vaccination history = one dose during outbreaks.
High-risk adults = serologic testing or presumptive second dose.
Conclusion
The measles resurgence underscores vaccination’s critical role but reveals nuanced immunity patterns. While antibody waning occurs, clinical protection remains robust for most two-dose recipients. Targeted boosting—rather than universal recommendations—optimizes resource use. Serologic testing of antibody levels for high-risk adults, catch-up doses for under-vaccinated cohorts, and emergency MMR administration during outbreaks when documentation is lacking are all described herein. Future research should clarify cell-mediated immunity’s role and develop standardized correlates of protection beyond IgG antibody titers.
I will cut and paste a massive number of additional references I used and that Perplexity crunched.
Measles is the canary in the coal mine for vaccine-preventable diseases. Strengthening childhood immunization systems, enhancing adult record-keeping, and addressing global vaccine equity remain paramount to preventing future outbreaks.
How are we doing on that lately?
Was this deeper dive worth it?





Here are those references and citations for the masochists among us!
https://www.nbcnews.com/health/health-news/childhood-vaccines-adults-booster-shots-measles-texas-what-know-rcna193197
https://pubmed.ncbi.nlm.nih.gov/36935110/
https://www.cdc.gov/vaccines/vpd/mmr/hcp/recommendations.html
https://pmc.ncbi.nlm.nih.gov/articles/PMC8189124/
https://www.cedars-sinai.org/newsroom/measles-makes-a-comeback-what-parents-need-to-measles-makes-a-comeback-what-parents-need-to-know/
https://www.npr.org/sections/shots-health-news/2025/02/21/nx-s1-5304458/measles-vaccine-booster-health
https://pmc.ncbi.nlm.nih.gov/articles/PMC6970218/
https://doh.wa.gov/sites/default/files/legacy/Documents/Pubs/348-479-MeaslesReferenceforProviders.pdf
https://www.who.int/news-room/fact-sheets/detail/measles
https://www.who.int/teams/immunization-vaccines-and-biologicals/diseases/measles
https://www.cdc.gov/vaccines/vpd/mmr/public/index.html
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae537/7874423
https://pmc.ncbi.nlm.nih.gov/articles/PMC7343595/
https://www.npr.org/2025/02/20/nx-s1-5302542/as-measles-cases-rise-its-not-just-kids-who-need-vaccines-some-adults-do-too
https://www.medrxiv.org/content/10.1101/2024.04.18.24306028v1
https://www.healthychildren.org/English/safety-prevention/immunizations/Pages/Protecting-Your-Baby-from-a-Measles-Outbreak-FAQs.aspx
https://pmc.ncbi.nlm.nih.gov/articles/PMC6414234/
https://news.uchicago.edu/big-brains-podcast-why-measles-resurging-and-rise-vaccine-hesitancy
https://www.ama-assn.org/delivering-care/public-health/long-covid-news-measles-texas-rsv-vaccine-moms-food-recalls-and-rural
https://www.news-medical.net/news/20240927/Study-shows-gradual-waning-of-MMR-vaccine-effectiveness-over-time.aspx
https://www.dshs.texas.gov/vaccine-preventable-diseases/vaccine-preventable-disease-conditions/measles-rubeola
https://www.science.org/doi/10.1126/science.aay6485
https://pmc.ncbi.nlm.nih.gov/articles/PMC6363159/
https://publichealth.jhu.edu/2025/what-to-know-about-measles-and-vaccines
https://www.dshs.texas.gov/news-alerts/measles-outbreak-feb-25-2025
https://www.khou.com/article/news/measles-booster-mmr-vaccine/285-553bfd35-a0d4-43a5-a4b7-9b22f9c22f51
https://www.cbsnews.com/news/measles-vaccine-booster-what-to-know/
https://www.houstonchronicle.com/news/houston-texas/trending/article/measles-vaccine-texas-outbreak-booster-20187132.php
https://www.pbs.org/newshour/show/west-texas-measles-outbreak-spreads-amid-vaccine-hesitancy-in-some-communities
More Citations:
https://www.news-medical.net/news/20240927/Study-shows-gradual-waning-of-MMR-vaccine-effectiveness-over-time.aspx
https://academic.oup.com/ofid/article/7/11/ofaa505/5932400
https://whyy.org/articles/measles-vaccine-booster-health/
https://pmc.ncbi.nlm.nih.gov/articles/PMC6970218/
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2782431
https://www.cidrap.umn.edu/measles/news-scan-sep-02-2020
https://www.nature.com/articles/s41467-023-37407-x
https://pmc.ncbi.nlm.nih.gov/articles/PMC10768653/
https://www.nbcnews.com/health/health-news/childhood-vaccines-adults-booster-shots-measles-texas-what-know-rcna193197
https://pmc.ncbi.nlm.nih.gov/articles/PMC8189124/
https://www.scielo.br/j/rimtsp/a/GvmM9bGk9GbtJxRJ674YHQn/
https://pubmed.ncbi.nlm.nih.gov/36935110/
https://pmc.ncbi.nlm.nih.gov/articles/PMC11663438/
https://pubmed.ncbi.nlm.nih.gov/35417025/
https://www.bmj.com/content/340/bmj.c1626
https://www.npr.org/sections/shots-health-news/2025/02/21/nx-s1-5304458/measles-vaccine-booster-health
https://www.medrxiv.org/content/10.1101/2024.04.18.24306028v1
https://pubmed.ncbi.nlm.nih.gov/39712819/
https://journals.plos.org/plosone/article?id=10.1371%2Fjournal.pone.0170257
https://www.ama-assn.org/delivering-care/public-health/long-covid-news-measles-texas-rsv-vaccine-moms-food-recalls-and-rural
https://www.cdc.gov/mmwr/preview/mmwrhtml/00041753.htm
https://www.healthdata.org/research-analysis/library/evaluating-scope-and-bias-population-level-measles-serosurveys
https://academic.oup.com/ofid/article/11/1/ofad700/7505490
https://academic.oup.com/jid/article/206/10/1542/858893
https://journals.asm.org/doi/10.1128/mbio.02628-20
https://www.thelancet.com/journals/lanpub/article/PIIS2468-2667(24)00181-6/fulltext
https://jamanetwork.com/journals/jamapediatrics/fullarticle/569784
https://academic.oup.com/jid/article/226/7/1127/6568034
https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciae537/7874423
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30442-4/abstract
Even More Citations:
https://hhs.iowa.gov/center-acute-disease-epidemiology/epi-manual/reportable-diseases/measles/controlling
https://www.chfs.ky.gov/agencies/dph/dehp/idb/Documents/KDPHMeaslesInvestigationGuide.pdf
https://www.cdc.gov/vaccines/vpd/mmr/public/index.html
https://www.healthychildren.org/English/safety-prevention/immunizations/Pages/Protecting-Your-Baby-from-a-Measles-Outbreak-FAQs.aspx
https://doh.wa.gov/sites/default/files/legacy/Documents/Pubs/348-479-MeaslesReferenceforProviders.pdf
https://www.cdph.ca.gov/Programs/CID/DCDC/CDPH%20Document%20Library/Immunization/Measles-Quicksheet.pdf
https://www.cdc.gov/vaccines/vpd/mmr/hcp/index.html
https://www.health.state.mn.us/communities/ep/han/2024/aug22measles.pdf
https://www.cdc.gov/vaccines/vpd/mmr/hcp/recommendations.html
http://publichealth.lacounty.gov/acd/procs/b73/DiseaseChapters/B73Measles.pdf
https://www.immunize.org/wp-content/uploads/catg.d/p4209.pdf
https://cdphe.colorado.gov/diseases-a-to-z/measles/measles-vaccination-recommendations
https://publichealth.jhu.edu/2025/what-to-know-about-measles-and-vaccines
https://kingcounty.gov/en/dept/dph/health-safety/disease-illness/measles/vaccine
https://www.immunize.org/ask-experts/topic/mmr/
https://libguides.mskcc.org/publichealth/MMRvaccination
https://www.cdph.ca.gov/Programs/CID/DCDC/CDPH%20Document%20Library/Immunization/HCWIZRecs.pdf
https://www.oregon.gov/oha/ph/DiseasesConditions/DiseasesAZ/Measles1/MeaslesVacRecom.pdf
https://www.npr.org/sections/shots-health-news/2025/02/21/nx-s1-5304458/measles-vaccine-booster-health
https://vaccine-schedule.ecdc.europa.eu/Scheduler/ByDisease?SelectedDiseaseId=8&SelectedCountryIdByDisease=-1
https://www.chop.edu/news/health-tip/measles-outbreak-how-protect-your-family
https://www.cdc.gov/measles/hcp/vaccine-considerations/index.html
https://www.dshs.texas.gov/news-alerts/measles-exposures-central-south-central-texas
https://www.cdc.gov/measles/vaccines/index.html
https://publications.aap.org/aapnews/news/31468/Nearly-100-infected-with-measles-amid-outbreak-in
https://www.cdc.gov/mmwr/preview/mmwrhtml/00041753.htm
https://immunizationdata.who.int/global/wiise-detail-page/vaccination-schedule-for-measles
https://pmc.ncbi.nlm.nih.gov/articles/PMC8189124/
https://www.health.state.mn.us/diseases/measles/hcp/control.html
https://www.michigan.gov/-/media/Project/Websites/mdhhs/Folder3/Folder46/Folder2/Folder146/Folder1/Folder246/Healthcare_Occ_Health_Measles_Guidance_3-28-19_FINAL.pdf?rev=06be3f7b25dc4838ad9c3f04497ae2ab
https://www.middlebury.edu/measles/proof-immunity-requirements-and-examples
https://www.cbsnews.com/news/measles-vaccine-booster-what-to-know/
https://www.cdc.gov/measles/travel/index.html
https://www.aafp.org/family-physician/patient-care/prevention-wellness/immunizations-vaccines/disease-pop-immunization/measles-vaccine.html
Thank you for this, Ryan. A public service.